Lately, there is an ongoing dietary debate – but debate may be the wrong word – given that discussion has tended to be one sided. This debate centers around a key component in our diet. Fat. Is it bad, or is it good? What about carbohydrates? An endless stream of diet fads, recommendations from health “professionals”, and research literature that often contradicts itself only muddy the water surrounding our discussion on what the optimal “diet” is to improve health, fight disease, and better our quality of life.
Many have heard the terms “low carb” and “keto” thrown around when discussion on what the optimal way to eat is. Additionally, there is no shortage of media and scientific coverage on the seeming shift in the way we are looking at the role of carbohydrates (namely, sugars) in the diet. We have concomitantly learned more about the harmful effects of dietary sugar, as well as the beneficial (or at least not as harmful as we once thought) effects of dietary fat. Given that the different types of fat (saturated, unsaturated, poly/mono-unsaturated, trans) all differentially effect our biology, there is a need for discussion and public health recommendation regarding the intake amounts and proportions of each in the diet. There is a shift – one advocating that we forget about an upper limit or recommendation on fat intake, and rather advise against high dietary carbohydrate consumption for general health but primarily for the prevention and treatment of metabolic disorders such as obesity and type II diabetes, as well as cardiovascular diseases, all of which have exploded in modern society.
Low-fat diets were once the foundation for nutrition recommendations. Unfortunately, these recommendations led to the increased consumption of “low fat” foods in which, paradoxically, the fat content was replaced with sugar to maintain a food’s palatability. While this may not be the only scapegoat for our current obesity epidemic –the “low fat is better” paradigm undoubtedly led to a higher consumption of refined carbohydrate. The thought that “fat makes you fat” once prevailed, and still lingers even to this day, yet more faintly. Indeed, it is now being shown that dietary carbohydrate observationally and causally associated cardiovascular disease risk factors.
Low-carb diets, now the predominantly advocated diet among most health and nutrition professionals for weight loss and health, purport many beneficial effects of this diet on blood lipid and glucose parameters as evidence of its superiority. We are beginning to see fat as more of a friend than a foe, however, the evidence is nowhere near conclusive as to what types and amounts of dietary should be emphasized and what types should be avoided (if any). The questions below appeared in a review titled “Dietary Fat: Friend or Foe” and is cited at the end for reference. It provides information and recommendations from leading nutritional experts in the field. It seems to provide some fantastic and generally moderate advice on dietary fat recommendations that can begin to replace our current understanding of what a healthy diet is and once was.
Did our previous national/international guidelines (to limit total dietary fat) contribute to the rise in obesity and other metabolic diseases, such as type II diabetes?
There is a strong link between diets high in refined carbohydrates (sugars) and obesity and type II diabetes. Recent but previous guidelines advocating a low-fat diet nudged the food industry and consumers toward a low-fat diet – that tended to be rich in sugars and other refined carbohydrates. Additionally, high-carbohydrate intake was advocated – if you can remember the 1992 Food Guide Pyramid – which recommended daily intake of 6-11 servings of bread, pasta, and grains!

E). The “low fat” foods that appeared in the market replaced their fat content with sugar to help maintain taste, structure, and texture. Unfortunately, sugar is not beneficial to health. Although the term “empty calorie” is no longer en vogue, replacing a dietary nutrient (fat) with something with no apparent dietary use had a net negative effect on health. Nonetheless, “low fat” foods were and are still marketed as “health foods.” Unfortunately, consumers also believed that “low-fat” and “fat-free” labels also meant that the foods were “low-calorie,” leading to an over-consumption of these foods. In addition to their sugar content, many foods that people switched over to during the 1970’s/80’s/90’s low-fat craze were high processed and refined – with the fat replaced by sugar, salt, and simple carbohydrates – and many essential nutrients taken out in the processing. The low-fat message also had other unanticipated consequences. Although saturated fat was the main target of recommendations – what occurred was a reduced consumption of ALL fats – including the healthy mono- and polyunsaturated fats.
How should we classify fat, as a “friend” or a “foe” based on its chemical structure (saturated and unsaturated) as well as the food source it is found in?
Trans Fats
Industrial trans fats are highly unhealthful due to the negative effects they exert on cardiovascular risk factors. Trans fat is NOT a natural part of our diet, and only has detrimental health consequences. The evidence that dietary trans fat increases the risk of CVD is well established – so all evidence points to complete elimination of this fat completely from the diet.
Note: On 16 June 2015, the FDA finalized its determination that trans fats are not generally recognized as safe, and set a three-year time limit for their removal from all processed foods. However, trans fats still appear in very small levels in meat and dairy products.

Unsaturated Fats (polyunsaturated/monounsaturated)
Polyunsaturated fatty acids (PUFAS) and mono
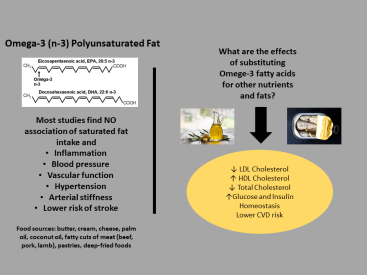
unsaturated fatty acids (MUFAS) are positively associated with health, and should be the predominate types of fat consumed in the diet. Unsaturated fats favorably affect disease risk by lowering many CVD risk factors – and diets rich in PUFA/MUFA are shown to be cardioprotective. Additionally, substituting saturated fat for PUFA has been shown to lower CVD risk and all-cause mortality (death from any possible cause). It should be noted, however, that many foods containing PUFA/MUFA also contain higher amounts of saturated fat.

Saturated Fats
When it comes to CVD risk, saturated fats have a relatively neutral (or no) effect. Overall, saturated fat does not raise cholesterol concentrations, but his depends on the “food matrix” it is consumed with or in. Thus, the food sources from which one gets their saturated fat need to be considered; we don’t eat nutrients, we eat foods. Rather than the total amount of saturated fat consumed – the proportion of fats may be the more important dietary factor.

What is the effect of increasing dietary fat on blood lipids and other disease risk factors. Is this a concern when prescribing a low-carb (high fat) diet?
Most importantly – the type of effect depends on the type of fat consumed, the baseline content of fat in the diet, metabolic status of the individual, and what the fat is replacing (protein or carbohydrate, different type of fat). For example – replacing carbohydrate (especially refined) with poly or monounsaturated fat will improve blood lipid profiles including lower triglycerides, and higher HDL cholesterol. However, simply just adding more fat (saturated) in the diet or replacing unsaturated with saturated fat will likely raise LDL and unfavorably affect blood lipids – and the food source of the additional fat is important. When PUFA’s are exchanged for equal calories with dietary carbohydrate, LDL, and triglycerides both decrease, and HDL increases. Additionally, saturated fat can have beneficial effects on blood lipids (HDL and triglycerides) when substituted for refined carbohydrate – but it also raises LDL, and may be overall detrimental compared to PUFA/MUFA. Trans fat, obviously, is the worst – as it decreased the “good” HDL and increases the “bad” LDL. One additional note on saturated fat and blood lipid effects. It has been shown that the increase in “bad” LDL due to intake of saturated fat may be the less harmful subtype of LDL; the large buoyant lipoproteins compared to the harmful small, dense lipoproteins).
Right now, there is no standard for what constitutes a “low carb” diet – and this term is too general and overly simplistic. Many authors of this review indicated they would prefer the avoidance of the term all together.
Should there be an upper limit (UL) on total fat intake as a % of daily calories?
One suggestion and for an upper limit may only be because it would promote the goal of achieving an otherwise balanced and healthy intake of other macro- and micro-nutrients to help stave of chronic disease risk. Some foods containing fiber and higher amounts of carbohydrate (fruits and vegetables) are an essential part of a healthy diet. Otherwise, there seems to be no basis for limiting the amount of total fat in the diet, an upper limit need not be established if one stays within their general caloric needs. In terms of what to encourage, levels of fat like those consumed in Mediterranean regions (40% of total energy intake) with a predominance of PUFA/MUFA should be recommended. In 2005, the U.S RDI for dietary fat was 35% of total energy intake (with >10% from saturated fat). Now, in the new 2015-2020 dietary guidelines for Americans, no upper limit is given. In terms of safety profile of high-fat diets, human populations have lived on periods of virtually zero carbohydrates, using fat as their primary energy source (some Inuit populations during the winter season). Ketogenic diets, with up to 80% total energy intake coming from fat, have been prescribed to children for epilepsy control for decades.
Should an upper limit on SATURATED fat be established? What about PUFA/MUFA?
An emphasis should be placed on limiting foods rich in trans/saturated fat intake to keep these subtypes low, however, limiting the threshold for these types of fats also limits one’s choices in food availability. What should be emphasized more is that most one’s dietary fat should come from PUFA/MUFA, since the saturated: unsaturated fat ration may be more important than total content of either. Most dietary fat should come from food sources high in PUFA/MUFA however, some foods that are rich in dietary saturated fat also contain many essential nutrients and should not be excluded from the diet. While no upper limit is stated, and no association has been shown between saturated fat intake and mortality, coronary heart disease, and type II diabetes – it is not explicitly recommended that one attempt to increase dietary intake of saturated fat directly.
What is the state of science regarding “personalized nutrition” – since the optimal diet for disease prevention and health may vary by individual genotype/phenotype?
Optimal diet prescription involves many interactions; among diet, physical activity, lifestyle factors, the environment, the epigenome, the microbiome, and the immune system. Needless to say, it is complex, and impossible to isolate a one or even a few variables. However, a better and more recent understand of the microbiome (“the gut”) may allow for better diet prescription for people who may be more susceptible to disease or sensitive to certain lifestyle/dietary interventions. One promising factor recently discovered is insulin secretion. Insulin is of major importance to metabolic health (its dysfunction leads to a variety of metabolic abnormalities including diabetes and possibly obesity). There seems to be a unique insulin secretion phenotype which may confer increased susceptibility to a high-carbohydrate diet. The ability to locate this genetic alteration in individuals would thus allow prescription of a low carb diet which may improve metabolic health and reduce obesity risk.
What are the most important health messages for preventing obesity?
Recently, the failure of the “calorie in-calorie out” approach to weight control as well as the “low fat diet” paradigm are being questioned. Conventional calorie restriction (diet) elicits unique physiological responses such as increased hunger and a slower metabolism which may predispose some people to regain the weight they initially lost. Additionally, there are biological drivers of weight gain that cannot simply be overridden by “eating less” as many diets suggest. While avoiding going into detail, the carbohydrate-insulin model of obesity/diabetes is providing us an understanding for why a higher-fat diet may be advantageous for weight control and disease prevention. (I’ll post some actions of insulin to accompany this post).
Another area of discussion should be to concern ourselves with food and whole dietary patterns instead of just individual nutrients. Additionally, consumers need to limit their consumption of ultra-processed foods and beverages (high in added sugars and refined carbohydrate) and focus on eating whole foods. Presentation of dietary control also matters. Instruction to NOT eat certain foods does not work well. Rather, a more effective approach to dietary control may be the suggestion to “try food X instead of food Y.”
Food preferences and eating habits beginning early in life – and so does obesity. There needs to be an awareness that obesity predisposition is driven by epigenetic mechanisms and that, once a child is “on course” to become obese, it is hard to reverse this due to powerful forces that may even occur before the child is conceived (i.e. the body fat % of the parents). We need to similarly think about the health of our infants and children. Preventing excessive weight gain during infancy by not introducing children to highly processed foods and allowing sufficient opportunities for physical activity and sleep patterns is important, as is fostering a strong family environment that encourages self-regulation. Teaching children the skills necessary to procure and prepare healthful meals should complement nutrition education in schools. This should be emphasized on par with drug avoidance and smoking cessation.
A key point to all dietary recommendations is that food should be enjoyed, and not feared. That being said. Modern society “over-enjoys” many of the foods that are leading us down a road of disease and disability. Dietary change begins at education, and proper dissemination of the current literature in the media and from scientists is the first step to solving the epidemic of metabolic dysregulation we are currently facing. Whether or not a focus on dietary fat intake while lowering carbohydrate intake will lead to a healthier public society, only time will tell. Discussions like this help further the public discourse and lead us closer to health. Without discussion like these? Well…fat chance.
Citation: Dietary Fat: Friend or Foe?